Questions and answers for medical professionals
Reviewer 1
Question1
There's plenty of controversy in the literature
about the importance of perforating veins in the pathogenesis of
varicosities. The author should explain his view of the
relationship of saphenopopliteal incompetence to varicose veins.
 Valvular insufficiency
is dynamic. Contraction of the so-called ‘peripheral heart’,
which is constituted by the leg muscles, generates the highest
venous pressure: up to 300 mm of mercury (6,7). This region,
which is of strategic importance for the correct functioning of
the venous circulation, contains about 100 perforating veins
(8), as well as the origin of the small saphenous vein, which
connect the superficial circulation with the deep circulation. Valvular insufficiency
is dynamic. Contraction of the so-called ‘peripheral heart’,
which is constituted by the leg muscles, generates the highest
venous pressure: up to 300 mm of mercury (6,7). This region,
which is of strategic importance for the correct functioning of
the venous circulation, contains about 100 perforating veins
(8), as well as the origin of the small saphenous vein, which
connect the superficial circulation with the deep circulation.
Question2
Ectatic reticular veins are often associated with a network
of
telangiectasia, explain.
 Telangiectasias form
when the ectatic reticular veins are no longer able to absorb
the rapid pressure increases caused by muscular contraction.
Telangiectasias may form even in the absence of visible
reticular veins if the capillary network is directly connected
to an incontinent perforating vein. Telangiectasias form
when the ectatic reticular veins are no longer able to absorb
the rapid pressure increases caused by muscular contraction.
Telangiectasias may form even in the absence of visible
reticular veins if the capillary network is directly connected
to an incontinent perforating vein.
Question3
Varicose veins routinely occur in the absence of
perforator insufficiency, explain.
 The functional anatomy
of the venous circulation in the lower limbs reveals that the
valvular insufficiency of the perforating veins and the ectasia
of the truncal veins, reticular veins, venules and
telangiectasias are, except for rare cases (mechanical
obstructions, traumas, arteriovenous fistulas, congenital
angiopathies, excessive functional performance (1), prolonged
exposure to heat or sun, cortisone application, radiodermatitis,
inflammation, chronic skin disorders, etc) due to congenital
miopragia of the vessel walls (1, 2, 3, 4, 5).The disorder is
sustained by perforating vessels which reveal their
insufficiency only when the patient runs or walks. Clearly then,
the insufficiency of even a small percentage of these vessels
can thwart any traditional treatment and give the erroneous
impression that ectatic veins can form without a hemodynamic
cause, apart from the causes listed above. The functional anatomy
of the venous circulation in the lower limbs reveals that the
valvular insufficiency of the perforating veins and the ectasia
of the truncal veins, reticular veins, venules and
telangiectasias are, except for rare cases (mechanical
obstructions, traumas, arteriovenous fistulas, congenital
angiopathies, excessive functional performance (1), prolonged
exposure to heat or sun, cortisone application, radiodermatitis,
inflammation, chronic skin disorders, etc) due to congenital
miopragia of the vessel walls (1, 2, 3, 4, 5).The disorder is
sustained by perforating vessels which reveal their
insufficiency only when the patient runs or walks. Clearly then,
the insufficiency of even a small percentage of these vessels
can thwart any traditional treatment and give the erroneous
impression that ectatic veins can form without a hemodynamic
cause, apart from the causes listed above.
Question4
"Hemodynamic" alterations follow the obliteration of
perforating
veins. This statement runs counter to a large body of opinions
suggesting that treatment of reticular veins? is important as a
first step in eradicating small vessels. Explain your theory.
 Even if obliterative
techniques are applied to perforating veins that appear
incontinent on color-flow doppler scanning, the problem will not
be solved and the progression of the disorder will not be
prevented. Indeed, hemodynamic alterations may be caused that
give rise to new capillary and venular ectasias; following the
obliteration of a perforating vein, the pressure on the
superficial venous circulation determined by other incontinent
perforating veins that cannot be revealed by means of the
instrumental examinations available may increase and be
manifested at the surface of the skin. It should be borne in
mind that visible ectatic vessels are the result of increased
pressure generated by valvular insufficiency;, some authors have
focused on treating the ectatic reticular veins; these, however,
represent the effect rather than the cause of the disorder. Even if obliterative
techniques are applied to perforating veins that appear
incontinent on color-flow doppler scanning, the problem will not
be solved and the progression of the disorder will not be
prevented. Indeed, hemodynamic alterations may be caused that
give rise to new capillary and venular ectasias; following the
obliteration of a perforating vein, the pressure on the
superficial venous circulation determined by other incontinent
perforating veins that cannot be revealed by means of the
instrumental examinations available may increase and be
manifested at the surface of the skin. It should be borne in
mind that visible ectatic vessels are the result of increased
pressure generated by valvular insufficiency;, some authors have
focused on treating the ectatic reticular veins; these, however,
represent the effect rather than the cause of the disorder.
Question5
Visible ectatic veins are the result of increased pressure
generated by valvular insufficiency", in point of fact there are
certainly at least several reasons why small vessels grow.
 Except for rare cases
(mechanical obstructions, traumas, arteriovenous fistulas,
congenital angiopathies, excessive functional performance (1),
prolonged exposure to heat or sun, cortisone application,
radiodermatitis, inflammation, chronic skin disorders, etc) due
to... Except for rare cases
(mechanical obstructions, traumas, arteriovenous fistulas,
congenital angiopathies, excessive functional performance (1),
prolonged exposure to heat or sun, cortisone application,
radiodermatitis, inflammation, chronic skin disorders, etc) due
to...
Question6
How does this novel solution produce "regenerative fibrosis
confined to the vascular tree?
 The wall fibrosis
induced by the endoluminal injection of the solution causes
thickening without disorganization of the wall; indeed, the
elastic fibers within the wall remain intact. The wall fibrosis
induced by the endoluminal injection of the solution causes
thickening without disorganization of the wall; indeed, the
elastic fibers within the wall remain intact.
Question7
What are the authors explanations for the molecular basis of
this very special type of fibrosis which seems too good to be
true.
 A non-buffered
solution of sodium salicylate and glycerol almost identical to
6% ******** has been tested A non-buffered
solution of sodium salicylate and glycerol almost identical to
6% ******** has been tested
on an ear vein of the rabbit, producing a clinical and
histological effect equivalent to that of chromic
glycerin (17). .”Chromic glycerin has been used for several
decades. We feel sure that the molecular basis
of the fibrosis that it causes, which is histologically
equivalent to that caused by ********, is available in the
literature.”
Question8
What in vivo studies have been carried out to determine
the precision of such fibrosis?
 Over the six years of
development of this technique, our utilization of the ********
solution Over the six years of
development of this technique, our utilization of the ********
solution
as steadily improved.
Question9
The assertion that this treatment restores the correct
conditions of blood flow and
pressure in the areas involved is not substantiated by any ofthe
studies presented in this paper. Discuss your laboratory
evaluations in detail.
 The fact that the
results obtained seem to be permanent is the most convincing
proof that functional integrity has been restored The fact that the
results obtained seem to be permanent is the most convincing
proof that functional integrity has been restored
Question10
Inflammatory matting occurring solely in areas of post
sclerotherapy
hyperpigmentation must be very rare. Why is
treatment of this type of matting unnecessary.
 The most difficult
cases of matting to treat are those with the highest pressure
and those that arise even The most difficult
cases of matting to treat are those with the highest pressure
and those that arise even
after modest pressure increases in a context of very marked
miopragia. If the former cases were treated with a
two-dimensional technique, matting would inevitably recur. The
rare cases of inflammatory matting resolve spontaneously
and do not require treatment. Inflammatory matting is clearly
visible in areas of post-sclerotherapy hyperpigmentation. For
the sake of simplicity, we have deleted the complex discussion
of inflammatory
matting following timedsurgical de-epithelialisation.. It is,
however, curious that most authors advise treating “inflammatory”
matting by injecting a sclerosing solution that causes further
inflammation”
Question11
Discuss the toxicology of salicylates and glycerol.
 The LD-50 of
intravenous polydocanol in the dog is 50 mg/kg. The LD-50 of
intravenous sodium salicylate in the dog is 562 g/Kg. In humans,
concentrations of salicylate greater than 200 mg/ml are regarded
as toxic. In mice, the LD-50 of glycerol administered
intravenously is 6.0 g/Kg. It should be stressed, however, that
the alkalization of ******** makes the absorption of sodium
salicylate at the systemic level practically nil The LD-50 of
intravenous polydocanol in the dog is 50 mg/kg. The LD-50 of
intravenous sodium salicylate in the dog is 562 g/Kg. In humans,
concentrations of salicylate greater than 200 mg/ml are regarded
as toxic. In mice, the LD-50 of glycerol administered
intravenously is 6.0 g/Kg. It should be stressed, however, that
the alkalization of ******** makes the absorption of sodium
salicylate at the systemic level practically nil
Question12
What studies have been carried out to assure safety when such
large volumes are
employed.
 The recommended limit
of 31.5 ml of 5% solution is determined by the duration of the
treatment session, which is about 30 minutes, and by the need to
keep well within the safety margins: 31.5 ml of solution
contains 27 ml of 6% ******** plus 4.5 ml of 1% lidocaine, which
is sufficient to treat even the most severe cases. During
experimentation of the method, we injected up to twice this
amount of solution (therefore 9 ml of lidocaine) without any
untoward effect. In that case, the amount of sodium salicylate
injected was 3.15 g and therefore still within the 3.6 g
limit of sodium salicylate used as a sclerosing solution (26). The recommended limit
of 31.5 ml of 5% solution is determined by the duration of the
treatment session, which is about 30 minutes, and by the need to
keep well within the safety margins: 31.5 ml of solution
contains 27 ml of 6% ******** plus 4.5 ml of 1% lidocaine, which
is sufficient to treat even the most severe cases. During
experimentation of the method, we injected up to twice this
amount of solution (therefore 9 ml of lidocaine) without any
untoward effect. In that case, the amount of sodium salicylate
injected was 3.15 g and therefore still within the 3.6 g
limit of sodium salicylate used as a sclerosing solution (26).
Question13
0.5 % policodanol is a very weak sclerosant which
would generally be ineffective for large varicose veins. Is this
a fair comparison?
 In traditional use,
the efficacy of the solutions has been seen to be very similar,
but the side effects are very different (see tabs 2, 3, 4). The
tolerability of ******** has proved to be far superior to that
of polydocanol (which used to be regarded as the best available
solution) and has opened the door In traditional use,
the efficacy of the solutions has been seen to be very similar,
but the side effects are very different (see tabs 2, 3, 4). The
tolerability of ******** has proved to be far superior to that
of polydocanol (which used to be regarded as the best available
solution) and has opened the door
to T.R.A.P.. Its efficacy is dose-dependent and therefore
increases as the dose increases, even
in large varicose veins”.
Question14
Compare and contrast the complications and efficacy of
0.5 % polidocanol and the solutions you employ.
Question15
"Potential for color-flow Doppler scanning is modest."
It is the opinion of most authorities that the assessment of the
degree of reflux achieved by color-flow Doppler is extremely
important for treating large veins.
 This examination is
important in the surgical treatment of large vessels, but is not
routine when three-dimensional regenerative phlebotherapy is to
be undertaken. Indeed, in the case of an exquisitely dynamic
disorder that is manifested when the patient is in movement, the
diagnostic potential of color-flow Doppler scanning is modest
This assertion is supported by Fig 2.27 of the treatise
Sclerotherapy by Mitchel P. Goldman (16), in which Doppler
examination of a patient suffering from a severe venous disorder
does not reveal any impairment of the sapheno-femoral or
sapheno-popliteal junctions, nor any incompetence of the
perforating veins. To our way of thinking, this is completely
absurd, in that even the tiniest telangiectasia is the outward
manifestation of the valvular incontinence of an underlying
vessel (18), except for those rare cases already mentioned. They
act exclusively on the full-blown aspects of the alteration in
venous circulation, while the disorder is sustained by
perforating vessels which reveal their insufficiency only when
the patient runs or walks. Clearly then, the insufficiency of
even a small percentage of these vessels, which cannot be
revealed by the instruments available, can thwart any
traditional treatment and give the erroneous impression that
ectatic veins can form without a hemodynamic cause, apart from
the causes listed above. This examination is
important in the surgical treatment of large vessels, but is not
routine when three-dimensional regenerative phlebotherapy is to
be undertaken. Indeed, in the case of an exquisitely dynamic
disorder that is manifested when the patient is in movement, the
diagnostic potential of color-flow Doppler scanning is modest
This assertion is supported by Fig 2.27 of the treatise
Sclerotherapy by Mitchel P. Goldman (16), in which Doppler
examination of a patient suffering from a severe venous disorder
does not reveal any impairment of the sapheno-femoral or
sapheno-popliteal junctions, nor any incompetence of the
perforating veins. To our way of thinking, this is completely
absurd, in that even the tiniest telangiectasia is the outward
manifestation of the valvular incontinence of an underlying
vessel (18), except for those rare cases already mentioned. They
act exclusively on the full-blown aspects of the alteration in
venous circulation, while the disorder is sustained by
perforating vessels which reveal their insufficiency only when
the patient runs or walks. Clearly then, the insufficiency of
even a small percentage of these vessels, which cannot be
revealed by the instruments available, can thwart any
traditional treatment and give the erroneous impression that
ectatic veins can form without a hemodynamic cause, apart from
the causes listed above.
Question16
"even the tiniest telangiectasia may or may not be a
manifestation of valvular
incompetence."
 The functional anatomy
of the venous circulation in the lower limbs reveals that the
valvular insufficiency of the perforating veins and the ectasia
of the truncal veins, reticular veins, venules and
telangiectasias are, The functional anatomy
of the venous circulation in the lower limbs reveals that the
valvular insufficiency of the perforating veins and the ectasia
of the truncal veins, reticular veins, venules and
telangiectasias are,
except for rare cases (mechanical obstructions, traumas,
arteriovenous fistulas, congenital angiopathies, excessive
functional performance (1), prolonged exposure to heat or sun,
cortisone application, radiodermatitis, inflammation, chronic
skin disorders, etc) due to congenital miopragia of the vessel
walls (1, 2, 3, 4, 5). to...
Question17
When the needle is no longer able to penetrate." Does
this mean the needle has become dull? Explain.
 When the needle is no
longer able to penetrate easily into the telangiectasias, it
must be replaced. When the needle is no
longer able to penetrate easily into the telangiectasias, it
must be replaced.
While a worn needle-tip is still able to penetrate a vein, it
will tend to displace rather than penetrate
telangiectasias
Question18
If resistance is"weak," is it possible to the degree of
resistance while encountered while injecting has as much to do
with the caliber of the vein injected as the degree of
incompetence? Explain.
 The three-dimensional
concept is clearly illustrated by the fact that 1 ml of 6%
solution may be injected into an isolated telangiectasia 2 mm in
length (12). This means that the pressure on the plunger of the
syringe is low and that the telangiectasia is the superficial
manifestation of the valvular incontinence of an underlying vein
that is directly connected to it (24) and which flows into the
deep circulation. The resistance felt on the plunger of the
syringe is therefore not related to the size of the
visible vessel injected, but to the size of the vessels
connected with it. The three-dimensional
concept is clearly illustrated by the fact that 1 ml of 6%
solution may be injected into an isolated telangiectasia 2 mm in
length (12). This means that the pressure on the plunger of the
syringe is low and that the telangiectasia is the superficial
manifestation of the valvular incontinence of an underlying vein
that is directly connected to it (24) and which flows into the
deep circulation. The resistance felt on the plunger of the
syringe is therefore not related to the size of the
visible vessel injected, but to the size of the vessels
connected with it.
Question19
What are the "areas of localized subcutaneous hardening"?
Histologically - is this scar tissue? Explain.
 These are small areas
of reactive hardening which disappear within a few weeks. No
histological examination of these has ever been carried out. These are small areas
of reactive hardening which disappear within a few weeks. No
histological examination of these has ever been carried out.
Question20
"Limit of 31.5cc of 6%" what is the LD-50 of this material
in animal studies.
How was this volume limit established?
 The recommended limit
of 31.5 ml of 5% solution is determined by the duration of the
treatment session, which is about 30 minutes, and by the need to
keep well within the safety margins: 31.5 ml of solution
contains 27 ml of 6% ******** plus 4.5 ml of 1% lidocaine, which
is sufficient to treat even the most severe cases. During
experimentation of the method, we injected up to twice this
amount of solution (therefore 9 ml of lidocaine) without any
untoward effect. In that case, the amount of sodium salicylate
injected was 3.15 g and therefore still within the 3.6 g limit
of sodium salicylate used as a sclerosing solution (26). The
LD-50 of intravenous polydocanol in the dog is 50 mg/kg. The
LD-50 of intravenous sodium salicylate in the dog is 562 g/Kg.
In humans, concentrations of salicylate greater than 200 mg/ml
are regarded as toxic. In mice, the LD-50 of glycerol
administered intravenously is 6.0 g/Kg. It should be stressed,
however, that the alkalization of ******** makes the absorption
of sodium salicylate at the systemic level practically nil The recommended limit
of 31.5 ml of 5% solution is determined by the duration of the
treatment session, which is about 30 minutes, and by the need to
keep well within the safety margins: 31.5 ml of solution
contains 27 ml of 6% ******** plus 4.5 ml of 1% lidocaine, which
is sufficient to treat even the most severe cases. During
experimentation of the method, we injected up to twice this
amount of solution (therefore 9 ml of lidocaine) without any
untoward effect. In that case, the amount of sodium salicylate
injected was 3.15 g and therefore still within the 3.6 g limit
of sodium salicylate used as a sclerosing solution (26). The
LD-50 of intravenous polydocanol in the dog is 50 mg/kg. The
LD-50 of intravenous sodium salicylate in the dog is 562 g/Kg.
In humans, concentrations of salicylate greater than 200 mg/ml
are regarded as toxic. In mice, the LD-50 of glycerol
administered intravenously is 6.0 g/Kg. It should be stressed,
however, that the alkalization of ******** makes the absorption
of sodium salicylate at the systemic level practically nil
Question21
explain why all patients receive antithrombotic therapy
and what are the products "which are also employed" and why are
they used.
 All patients require
anti-platelet therapy in order to limit intravascular blood
accumulation and venous All patients require
anti-platelet therapy in order to limit intravascular blood
accumulation and venous
thromboses.
Question23
results - Perhaps the author would entertain the
possibility that not all telangiectasia occur on the basis of
reduction of hemodynamic pressure.Visible ectatic veins are the
result of increased pressure
generated by valvular insufficiency", in point of fact there are
certainly at least several reasons why small vessels grow.
 Except for rare cases
(mechanical obstructions, traumas, arteriovenous fistulas,
congenital angiopathies, excessive functional performance (1),
prolonged exposure to heat or sun, cortisone application,
radiodermatitis, inflammation, chronic skin disorders, etc) due
to... Except for rare cases
(mechanical obstructions, traumas, arteriovenous fistulas,
congenital angiopathies, excessive functional performance (1),
prolonged exposure to heat or sun, cortisone application,
radiodermatitis, inflammation, chronic skin disorders, etc) due
to...
Question24
Discussion - If T.R.A.P. acts on vessels that are not
obviously pathological, animal studies could be used to
determine the specifics of its action. Were they employed?
 A non-buffered
solution of sodium salicylate and glycerol almost identical to
6% ******** has been tested on an ear vein of the rabbit,
producing a clinical and histological effect equivalent to that
of chromic glycerin (17) A non-buffered
solution of sodium salicylate and glycerol almost identical to
6% ******** has been tested on an ear vein of the rabbit,
producing a clinical and histological effect equivalent to that
of chromic glycerin (17)
Question25
Do the authors worry about the injection of this
solution into periocular areas where the effect of "regenerative
fibrosis" may be unpredictable.What is the rationale for
injecting telangiectasia on the face? Normalization of reflux?
explain.
 Facial telangiectasias,
if they can be injected, are part of a three-dimensional
disorder. The reduction in the overall volume of the veins
reduces the hemodynamic pressure on the capillary-papillary
plexus, thereby enabling a more rapid and stable result to be
achieved through subsequent treatment by physical means), which
is always Facial telangiectasias,
if they can be injected, are part of a three-dimensional
disorder. The reduction in the overall volume of the veins
reduces the hemodynamic pressure on the capillary-papillary
plexus, thereby enabling a more rapid and stable result to be
achieved through subsequent treatment by physical means), which
is always
necessary in this region in order to eliminate the vessels
completely. By contrast, complete elimination of telangiectasias
of the lower limbs, in our experience, does not require the use
of any physical technique.The solution injected into the vessels
of the cheek mainly flows toward the mandible; only in the nasal
and palpebral
regions, therefore, do we apply compression during injection of
the angular vein at the internal corner of the eyelid. Although
the angular vein is normally valved, this maneuver is
recommended on account of the possibility of anatomical
alterations of the vessel. It should be borne in mind that the
effect of ******** is predictable
Question26
The use of small quantities of two drops into spider
veins. Aren't telangiectasia spider veins (naevi no vein)?
Explain.
 Spider naevi are
arterial formations and should be injected with only a few drops
of 6% ******** Spider naevi are
arterial formations and should be injected with only a few drops
of 6% ********
Question27
Histologic section of skin, right "Has restored uniform
wall thickness", is this the biopsy of the same vein? Explain.
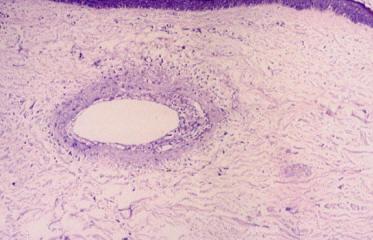
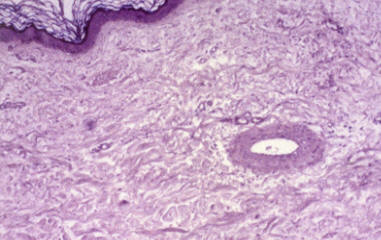
 (Right) Histological
section of skin. The same patient, the same area and a vein of
the same size seen after (Right) Histological
section of skin. The same patient, the same area and a vein of
the same size seen after
treatment with 6% ********.
Question28
Matting may represent an exaggerated form of
vascular remodeling which can occur as a consequence of trauma
and the release of inflammatory cytokines unrelated to "gateways
and venous reflux".
 The most difficult
cases of matting to treat are those with the highest pressure
and those that arise even The most difficult
cases of matting to treat are those with the highest pressure
and those that arise even
after modest pressure increases in a context of very marked
miopragia. If the former cases were treated
with a two-dimensional technique, matting would inevitably recur.
The rare cases of inflammatory
matting resolve spontaneously and do not require treatment.Only
hemodynamic matting is of phlebological interest. Inflammatory
matting, together with pigmentations, indicates that the type
and concentration of the solution are inappropriate.
Comment to Author of Reviewer 1
 This is a provocative and perhaps seminal article which
contains
a large number of theories and potential patient risks which
have not been assessed in an objective and scientific manner. This is a provocative and perhaps seminal article which
contains
a large number of theories and potential patient risks which
have not been assessed in an objective and scientific manner.
Varicose veins and telangiectasia probably occur on a
multifactorial basis and this approach may be one of many which
have potential importance but may not stand the test of time and
comparison to other evolving technologies.
Reviewer 2
Question28
the authors state "the valvular and ostial
incontinence of the great saphenous vein is of only marginal
importance." if that is the case, how do the authors
explain
the functional and cosmetic improve offered by endovenous
saphenous ablation procedures?
 By contrast, the
valvular and ostial incontinence of the great saphenous vein is
of marginal importance with regard to pressure, , since the
hydrostatic pressure at the ankle is 80/100 mm of mercury
regardless of whether the valves are continent or not (9,10).
The valvular incontinence of the largest superficial vein has a
clinical significance only if it is associated to
saphenopopliteal incompetence and valvular insufficiency of the
perforating veins. Indeed, cases have been observed of subjects
born without valves in the great saphenous vein who do not
manifest any disorder, while efficient valves have been found in
the external iliac vein of subjects suffering from varicose
veins (11)Saphenectomy is certainly three-dimensional, but it
does not respect the anatomical and functional integrity of the
circulation. The improvement seen in patients following ablation
of the great saphenous vein largely depends on the ligature of
the major perforating veins and on the obliteration of the
perforating veins that are connected to it. Surgical ablation of
the saphenous vein, however, is an incomplete treatment which
yields inconsistent results (12) and, from our point of view,
cannot be adopted as the therapy of choice for insufficiency of
the venous circulation in the lower limbs, in the majority of
cases. Saphenectomy yields long-lasting, good-quality results
only in those patients in whom the residual perforating veins
are continent. Even in such cases, however, the developmental
aspects of the varicose disorder determined by the miopragia of
the vessel walls cannot be avoided. While fine-tuning T.R.A.P.,
we have noticed that saphenectomy patients need more sessions of
phlebotherapy in order to achieve optimum results. We may
hypothesize that this is due to the anatomical-functional
alterations caused by the operation itself. With regard to
ambulatory phlebectomy, until now this has been justified only
by the absence of residual pigmentation. Obviously, the
availability of a solution that does not generate permanent
post-sclerotherapy pigmentation relegates this operation to the
level of a second choice. By contrast, the
valvular and ostial incontinence of the great saphenous vein is
of marginal importance with regard to pressure, , since the
hydrostatic pressure at the ankle is 80/100 mm of mercury
regardless of whether the valves are continent or not (9,10).
The valvular incontinence of the largest superficial vein has a
clinical significance only if it is associated to
saphenopopliteal incompetence and valvular insufficiency of the
perforating veins. Indeed, cases have been observed of subjects
born without valves in the great saphenous vein who do not
manifest any disorder, while efficient valves have been found in
the external iliac vein of subjects suffering from varicose
veins (11)Saphenectomy is certainly three-dimensional, but it
does not respect the anatomical and functional integrity of the
circulation. The improvement seen in patients following ablation
of the great saphenous vein largely depends on the ligature of
the major perforating veins and on the obliteration of the
perforating veins that are connected to it. Surgical ablation of
the saphenous vein, however, is an incomplete treatment which
yields inconsistent results (12) and, from our point of view,
cannot be adopted as the therapy of choice for insufficiency of
the venous circulation in the lower limbs, in the majority of
cases. Saphenectomy yields long-lasting, good-quality results
only in those patients in whom the residual perforating veins
are continent. Even in such cases, however, the developmental
aspects of the varicose disorder determined by the miopragia of
the vessel walls cannot be avoided. While fine-tuning T.R.A.P.,
we have noticed that saphenectomy patients need more sessions of
phlebotherapy in order to achieve optimum results. We may
hypothesize that this is due to the anatomical-functional
alterations caused by the operation itself. With regard to
ambulatory phlebectomy, until now this has been justified only
by the absence of residual pigmentation. Obviously, the
availability of a solution that does not generate permanent
post-sclerotherapy pigmentation relegates this operation to the
level of a second choice.
Question29
How is "********" different from other sclerosants?
How
does
it achieve non-obliterative regeneration of the vessels?
Is
it
the innate property of the "********" solution used?
Or is
it
simply the lower concentration used?
If it is just lower
concentration that makes it non-obliterative, then can the same
procedure be performed using more commonly accepted sclerosants,
such as Sotradecyl or polidocanol?
 We do not claim that
the vessel fibrosis caused by ******** is histologically
different from that caused by other chemical solutions. For what
concerns the ability to consistently induce efficacious fibrosis,
we do not know whether this feature is exclusive to ******** or
whether it can be achieved by means of other solutions. At
present, we know that chromic glycerin is able to produce a
similar degree of fibrosis, though we have never considered the
possibility of injecting large amounts of this solution. With
regard to exclusively water-based solutions, we believe that, if
suitably diluted, they may be able to exert a “regenerative”
effect. However, we do not know whether they are able to
maintain this effect in depth, on starting from the superficial
vessels, or whether they would immediately become diluted and
therefore lose all efficacy. We do not claim that
the vessel fibrosis caused by ******** is histologically
different from that caused by other chemical solutions. For what
concerns the ability to consistently induce efficacious fibrosis,
we do not know whether this feature is exclusive to ******** or
whether it can be achieved by means of other solutions. At
present, we know that chromic glycerin is able to produce a
similar degree of fibrosis, though we have never considered the
possibility of injecting large amounts of this solution. With
regard to exclusively water-based solutions, we believe that, if
suitably diluted, they may be able to exert a “regenerative”
effect. However, we do not know whether they are able to
maintain this effect in depth, on starting from the superficial
vessels, or whether they would immediately become diluted and
therefore lose all efficacy.
Question30
The authors have not demonstrated how this new procedure is
non-obliterative. Only one histological comparison was
offered. But it is not clear that after multiple extensive injection
sessions, that the veins are not obliterated, as they are in
sclerotherapy.
 The ability to cause
controlled, predictable fibrosis, which is a feature of ********,
can be verified by observing the superficial vessels. If small
amounts of 6% solution are injected into a vein, the caliber of
the vein will be reduced within a week. Further injection into
the same vein will result in a further reduction in caliber
within another week, and so on until the vein is no longer
visible. If, by contrast, we inject enough of the solution to “regenerate”
the underlying vessels, the resulting reduction in hemodynamic
pressure will allow the vein to shrink until it is no longer
visible after only one treatment session. This does not mean
that the vein has been obliterated. Obliteration is accompanied
by evident inflammation and by sclerotic hardening of the
vessel. The injection of ******** does not have such effects,
even in large-diameter reticular veins. Intravascular blood
accumulation may occasionally occur during T.R.A.P.. However,
even in such cases, the vessel is not obliterated completely.
Indeed, if a vessel containing an accumulation of blood (and
therefore already treated) is erroneously re-treated, it will
still be able to take in a fair amount of solution, and the only
indication that a vessel containing an accumulation has been
injected will be the quality of the blood that seeps from the
injection site. The ability to cause
controlled, predictable fibrosis, which is a feature of ********,
can be verified by observing the superficial vessels. If small
amounts of 6% solution are injected into a vein, the caliber of
the vein will be reduced within a week. Further injection into
the same vein will result in a further reduction in caliber
within another week, and so on until the vein is no longer
visible. If, by contrast, we inject enough of the solution to “regenerate”
the underlying vessels, the resulting reduction in hemodynamic
pressure will allow the vein to shrink until it is no longer
visible after only one treatment session. This does not mean
that the vein has been obliterated. Obliteration is accompanied
by evident inflammation and by sclerotic hardening of the
vessel. The injection of ******** does not have such effects,
even in large-diameter reticular veins. Intravascular blood
accumulation may occasionally occur during T.R.A.P.. However,
even in such cases, the vessel is not obliterated completely.
Indeed, if a vessel containing an accumulation of blood (and
therefore already treated) is erroneously re-treated, it will
still be able to take in a fair amount of solution, and the only
indication that a vessel containing an accumulation has been
injected will be the quality of the blood that seeps from the
injection site.
Question31
Properly performed sclerotherapy is already very similar to
the treatment process outlined by the patients. Most
phlebologist advocate treatment of veins in a logical
progression, from the largest to the smaller veins. From
the
highest point of reflux to the lowest. Therefore, all
layers of
the superficial venous system are treated. In this context,
properly performed sclerotherapy is already "three-dimensional",
not "two-dimensioanl", as suggested by the authors.
 We believe that
T.R.A.P. has the potential to be widely used. Indeed, alongside
the rigorously obliterative approach, there exists an
orientation towards a milder form of sclerotherapy that utilizes
the minimum effective concentration of solution (26). Clearly, a
form of sclerotherapy that is by definition obliterative cannot
completely embrace our philosophy. Indeed, “obliterating” the
entire superficial and perforating circulation is unthinkable;
it can, however, be “regenerated”. The notion that treatment
should be carried out progressively from the largest to the
smallest veins is not in line with the concepts we adopt. In our
view, what is important is the pressure, not the size. Indeed,
size may be determined by wall weakness in a single vessel. Even
telangiectasias are frequently used as gateways for the “regeneration”
of perforating veins. We do not consider the perforating veins
to be part of the superficial circulation. We believe that
T.R.A.P. has the potential to be widely used. Indeed, alongside
the rigorously obliterative approach, there exists an
orientation towards a milder form of sclerotherapy that utilizes
the minimum effective concentration of solution (26). Clearly, a
form of sclerotherapy that is by definition obliterative cannot
completely embrace our philosophy. Indeed, “obliterating” the
entire superficial and perforating circulation is unthinkable;
it can, however, be “regenerated”. The notion that treatment
should be carried out progressively from the largest to the
smallest veins is not in line with the concepts we adopt. In our
view, what is important is the pressure, not the size. Indeed,
size may be determined by wall weakness in a single vessel. Even
telangiectasias are frequently used as gateways for the “regeneration”
of perforating veins. We do not consider the perforating veins
to be part of the superficial circulation.
Question32
The authors also claim that sclerotherapy is only performed
on visible and pathological veins (Table 1). This is not
correct. Often times, in order to treat visible
telangiectasia,
the underlying feeding reticular veins must be eliminated first
in sclerotherapy.
 Only clearly
pathological vessels are injected and the reticular veins that
are connected to ectatic venules Only clearly
pathological vessels are injected and the reticular veins that
are connected to ectatic venules
and telangiectasias. Reticular veins connected to
telangiectasias are normally visible to the naked eye because
they are ectatic.
Question 33
When considering complications, matting and pigmentation
still is a problem with this procedure, similar to
sclerotherapy. I do not feel that the authors have
demonstrated
a better safety profile.
 Over the six years of
development of this technique, our utilization of the ********
solution has steadily improved. For instance,
de-epithelialization no longer occurs. Moreover, cases of
pigmentation are rare, limited to the injection sites and
short-lived; from the esthetic point of view they are therefore
irrelevant and, after the first session, are always avoidable.
With regard to matting, we maintain that the most critical areas
are the internal region of the knee and the lateral region of
the thigh. Transillumination, which we have only been using for
the past year, has proved very useful in completing the
regenerative action in these areas and has enabled us to
minimize this complication, which, moreover, normally resolves
easily. Over the six years of
development of this technique, our utilization of the ********
solution has steadily improved. For instance,
de-epithelialization no longer occurs. Moreover, cases of
pigmentation are rare, limited to the injection sites and
short-lived; from the esthetic point of view they are therefore
irrelevant and, after the first session, are always avoidable.
With regard to matting, we maintain that the most critical areas
are the internal region of the knee and the lateral region of
the thigh. Transillumination, which we have only been using for
the past year, has proved very useful in completing the
regenerative action in these areas and has enabled us to
minimize this complication, which, moreover, normally resolves
easily.
Question34
The authors admit that the proposed limit of the ********
solution of 31.5ml is based solely by the duration of the
treatment session. This is neither a scientific nor safe
method
to establish a such guideline.
 The recommended limit
of 31.5 ml of 5% solution is determined by the duration of the
treatment session, which is about 30 minutes, and by the need to
keep well within the safety margins: 31.5 ml of solution
contains 27 ml of 6% ******** plus 4.5 ml of 1% lidocaine, which
is sufficient to treat even the most severe cases. During
experimentation of the method, we injected up to twice this
amount of solution (therefore 9 ml of lidocaine) without any
untoward effect. In that case, the amount of sodium salicylate
injected was 3.15 g and therefore still within the 3.6 g limit
of sodium salicylate used as a sclerosing solution (26). )
. The LD-50 of intravenous polydocanol in the dog is 50 mg/kg.
The LD-50 of intravenous sodium salicylate in the dog is 562
g/Kg. In humans, concentrations of salicylate greater than 200
mg/ml are regarded as toxic. In mice, the LD-50 of glycerol
administered intravenously is 6.0 g/Kg. It should be stressed,
however, that the alkalization of ******** makes the absorption
of sodium salicylate at the systemic level practically nil The recommended limit
of 31.5 ml of 5% solution is determined by the duration of the
treatment session, which is about 30 minutes, and by the need to
keep well within the safety margins: 31.5 ml of solution
contains 27 ml of 6% ******** plus 4.5 ml of 1% lidocaine, which
is sufficient to treat even the most severe cases. During
experimentation of the method, we injected up to twice this
amount of solution (therefore 9 ml of lidocaine) without any
untoward effect. In that case, the amount of sodium salicylate
injected was 3.15 g and therefore still within the 3.6 g limit
of sodium salicylate used as a sclerosing solution (26). )
. The LD-50 of intravenous polydocanol in the dog is 50 mg/kg.
The LD-50 of intravenous sodium salicylate in the dog is 562
g/Kg. In humans, concentrations of salicylate greater than 200
mg/ml are regarded as toxic. In mice, the LD-50 of glycerol
administered intravenously is 6.0 g/Kg. It should be stressed,
however, that the alkalization of ******** makes the absorption
of sodium salicylate at the systemic level practically nil
Comments to Author of Reviewer 2
 I congratulate the authors on this innovative paradigm in
the treatment of venous insufficiency. But I feel that in
promoting this new concept, the authors have understated, or
simply overlooked the benefits of properly performed
sclerotherapy and other well-established procedures:Clearly this
procedure is still in its infancy. I congratulate the authors on this innovative paradigm in
the treatment of venous insufficiency. But I feel that in
promoting this new concept, the authors have understated, or
simply overlooked the benefits of properly performed
sclerotherapy and other well-established procedures:Clearly this
procedure is still in its infancy.
As the authors state, only when it is performed more widely and
in more extreme
cases can we understand the limits and the long term benefits.
A more revealing study would be a side-by-side comparison
between sclerotherapy and "phlebotherapy". As it is now, I
doubt this information will change the clinical practice of most
phlebologists. But the value of this manuscript is still
undeniable; this new "regenerative" treatment concept encourages
phlebologists to view the treatment of venous reflux from an
entirely different angle.
Re: RE : [vasculab] R: More physiological appraisal [dicember
2007]
vasculab@yahoogroups.com
 Capurro)
Capurro)
In a previous e-mail, I asked colleagues where they thought the
problem of
venous insufficiency lay. Indeed, in order to solve a problem, I
think the
first thing to do should be to agree on what the origin of the
problem is.
I probably made a mistake in sending the message, which was not
delivered.
Please forgive me for interfering, but this question intrigues
me. In order
to explain my thoughts in simple terms, let me start from the
observations
made by Franceschi.
According to Franceschi...
Franceschi)
...the danger is that we might “look at the smoke
(varices) and ignore the fire (haemodynamic condition) beneath
it”. His
Theory and Practice were described in a book that is still
available in
French, English and Italian: Claude Franceschi: cure CHIVA :
http://www.editions-armancon.fr/ , in which the author states: “When
drugs
repair walls and venous valves, CHIVA will disappear.”
 Capurro)
Capurro)
Franceschi locates the problem in the walls of the veins. But of
which
veins ? In other words: where is the fire? Clearly, not in the
superficial
vessels, which merely manifest the effect of the disease: “the
smoke”, as
Franceschi puts it.
If this is correct, obliterating or removing the effect of the
disease does
not seem to be a good idea, as it does not address the cause;
moreover, it
eliminates the “escape valve” of the underlying hypertension (as
well as
subverting the natural anatomy and physiology of the circulation,
of
course).
Franceschi locates the problem in the walls of the veins. But
which veins ?
Clearly, not the great saphenous vein (the innocence of which
emerges from
the literature; indeed, many individuals are born without valves
in the
great saphenous vein and femoral vein, and yet they do not
develop varices).
Rather, the problem lies in the veins that cannot be seen: the
perforating
veins, which are subjected to the highest haemodynamic pressure.
It seems
to me that, in any system of pipes, what is important is not the
dimensions
of the vessels, but the pressure, which is determined by the
weakness of
their walls. Indeed, in the leg, the pressure may reach 300 mmHg!
If all
of this is true, what happens? The walls of the perforating
vessels dilate
when the patient walks, the valves cannot withstand the pressure,
and an
anomalous pressure is exerted on the superficial circulation,
the vessels of
which become dilated. If the walls of the reticular veins are
particularly
weak, classic varices will develop; if the reticular veins can
withstand the
pressure, then the venules will dilate; if the venules can
withstand the
pressure, then the telangiectasias will dilate. These are three
aspects of
the same phenomenon. Obviously, an insufficient perforating
vessel may be
manifested on the skin in the form of an isolated telangiectasia.
If these
concepts are correct, it is necessary to strengthen the walls of
the
perforating veins, where the anomalous pressure originates.
Naturally, the
entire perforating circulation must be treated; it is irrational
to think
that wall miopragia should be located in a small area of the
limb. The
whole limb must be treated. How? The simplest approach is to
follow the
same pathway in the opposite direction. This involves injecting
a solution
that is not obliterating but “regenerative” (regeneration =
restoration of
function) into the vessels that are visible to the naked eye and
on
trans-illumination, and pressing it into the perforating veins (most
of
which cannot be visualised by colour Echo Doppler). The
perforating veins
will be strengthened, will shrink slightly, and will once again
become
continent. In this way, the anomalous pressure exerted on the
superficial
circulation will be relieved, and the vessels will disappear
permanently
from view. For what concerns the valves, once they have been
destroyed,
they cannot be restored. It is therefore advisable to avoid
destroying the
valves through the use of improper methods, to prevent phlebitis,
and, in
subjects with a familial predisposition, to undertake preventive
measures
before vessels visible to the naked eye develop.
With best regards,
Sergio Capurro
Inviato: lunedì 3 dicembre 2007 6.27
A: vasculab@yahoogroups.com
Simka)
Uzytkownik Sergio Capurro <sergio.capurro@fastwebnet.it> napisal:
Let me comment on that,
My opinion is that pathophysiology of varicose veins cannot be
explained exclusively by means
of haemodynamics. Not regarding the cellular and molecular
aspects of this pathology (yet,
affected by impaired haemodynamics) is the easiest way to create
a new dogma in phlebology.
Marian Simka
Franceschi)
Dear Marian, I agree with you about neo angigenesis but which is
the trigger? Why not
haemodynamic phenomenon? If it is, suppressing the haemodynamic
trigger should avoid neo
angiogenesis. Haemodynamic is not a dogma but a necessary ( even
if not sufficient) cause of
venous insufficiency.
Regards
Claude Franceschi
Simka)
Dear Claude,
I agree with you in the point that likely it is haemodynamics,
which triggers all these events.
However, in a current phlebology there exists macroscopic
approach (surgery, diagnostic
imaging, haemodynamic assessment, etc.) and microscopic approach
(genetics, cell biology, etc).
The both could be potentially regarded as two sides of the same
coin (like Newton’s
mechanics and quantum mechanics in the physics). Hopefully,
investigations focused on the role
of a pathology in a macrophlebology on microphlebological level,
and vice versa, could explain
some not yet solved problems.
Best regards
Marian Simka
 Capurro)
Capurro)
Cellular and molecular aspects concern miopragia, which, as we
have said, is the cause of
venous wall dilation in subjects with a familial predisposition
to varicose disease. As yet,
we cannot act upon this familial disposition; we can only make
recommendations regarding
lifestyle and diet. There is no pill that a mother can take
during pregnancy in order to
eliminate the predisposition to varicose veins in her child.
By contrast, when ectatic vessels begin to manifest themselves –
even those visible only by
means of transillumination – we can functionally correct the
congenital and acquired cellular
and molecular aspects of the vessel walls, which, as they dilate,
give rise to valvular
insufficiency.
In order to understand the concept of the regenerative treatment
of the superficial and
perforating circulation, it must be borne in mind that even a
tiny telangiectasia (except for
rare cases of mechanical obstructions, traumas, arteriovenous
fistulas, congenital
angiopathies, prolonged exposure to heat or sun, cortisone
application, radiodermatitis,
inflammation, chronic skin disorders, etc.) is caused by
valvular insufficiency.
In reality, essential varices do not exist (this concept stems
from inefficacious diagnosis).
Our intervention aims to re-establish proper hemodynamics by
exerting an effect, which is
logically molecular and cellular, on the walls of the vessels
responsible (perforating veins);
in this way, the vessels shrink, are strengthened and become
continent once more, without
losing their elastic properties. The procedure must be carried
out on the entire superficial
and perforating circulation in order to reduce all anomalous
pressures. The pumps must recover
their functional status, without leaks, especially where the
pressure is highest.
If the smallest telangiectasia is caused by valvular
insufficiency, the functional result and
the aesthetic result evidently coincide. For this reason, our
treatment terminates when there
are no longer any vessels visible to the naked eye or on
transillumination. This means that
the entire circulation has been “cured” and that the result will
remain permanent.
Best regards
Sergio Capurro
|